
Disparities in healthy food access are well documented in cross-sectional studies in communities across the United States. However, longitudinal studies examining changes in food environments within various neighborhood contexts are scarce. In a sample of 142 census tracts in four low-income, high-minority cities in New Jersey, United States, we examined the availability of different types of food stores by census tract characteristics over time (2009–2017). Outlets were classified as supermarkets, small grocery stores, convenience stores, and pharmacies using multiple sources of data and a rigorous protocol. Census tracts were categorized by median household income and race/ethnicity of the population each year. Significant declines were observed in convenience store prevalence in lower- and medium-income and majority black tracts (p for trend: 0.004, 0.031, and 0.006 respectively), while a slight increase was observed in the prevalence of supermarkets in medium-income tracts (p for trend: 0.059). The decline in prevalence of convenience stores in lower-income and minority neighborhoods is likely attributable to declining incomes in these already poor communities. Compared to non-Hispanic neighborhoods, Hispanic communities had a higher prevalence of small groceries and convenience stores. This higher prevalence of smaller stores, coupled with shopping practices of Hispanic consumers, suggests that efforts to upgrade smaller stores in Hispanic communities may be more sustainable.

Introduction
The US Preventive Services Task Force recommends that all patients be screened for obesity and, if needed, be provided weight-loss advice. However, the prevalence of such advice is low and varies by patient demographics. This study aimed to describe the determinants of receiving weight-loss advice among a sample with a high proportion of low-income, racial/ethnic minority individuals.
Methods
Data were collected from a telephone survey of 1,708 households in 2009 and 2010 in 5 cities in New Jersey. Analyses were limited to 1,109 overweight or obese adults. Multivariate logistic regression determined the association of participants’ characteristics with receiving weight-loss advice from their health care provider. Two models were used to determine differences by income and insurance status.
Results
Of all overweight or obese respondents, 35% reported receiving advice to lose weight. Receiving advice was significantly associated with income in multivariate analysis. Compared with those with an income at or below 100% of the federal poverty level (FPL), those within 200% to 399% of the FPL had 1.60 higher odds of receiving advice (P = .02), and those with an income of 400% or more of the FPL had 1.73 higher odds of receiving advice (P = .03). The strength of the association did not change after adjusting for health insurance.
Conclusion
Income is a significant predictor of whether or not overweight or obese adults receive weight-loss advice after adjustment for demographic variables, health status, and insurance status. Further work is needed to examine why disparities exist in who receives weight-loss advice. Health care providers should provide weight-loss advice to all patients, regardless of income.

Many factors influence children’s health behaviors and health outcomes. The Social Ecological Model (SEM) groups these factors into interactive layers, creating a framework for understanding their influence and for designing interventions to achieve positive change. The layers of influence in the SEM include individual, interpersonal, organizational, community, and policy factors.


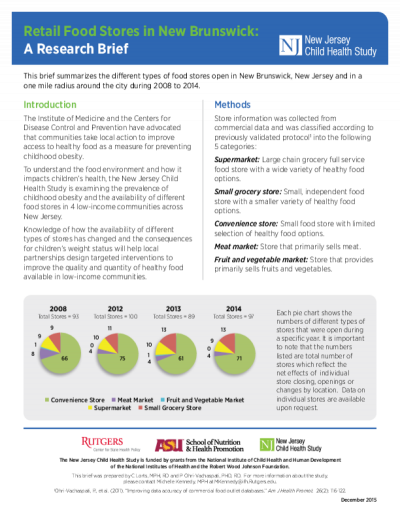
This brief summarizes the different types of food stores open in New Brunswick, New Jersey and in a one mile radius around the city during 2008 to 2014.

Many factors influence children’s health behaviors and health outcomes. The Social Ecological Model (SEM) groups these factors into interactive layers, creating a framework for understanding their influence and for designing interventions to achieve positive change. The layers of influence in the SEM include individual, interpersonal, organizational, community, and policy factors (see figure). The New Jersey Child Health Study (NJCHS) was designed to examine how specific layers of the SEM, particularly food and physical activity environments in schools and communities, affect obesity outcomes in children

With more than 19 million confirmed COVID-19 cases across the United States1 and over 500,000 in Arizona as of December 2020, the ongoing pandemic has had devastating impacts on local, national, and global economies. Prior to the pandemic (February 2020), based on U.S. Bureau of Labor Statistics data, the unemployment rate in Arizona was 6.5%, compared to 4.9% at the national level.3 Since the beginning of the COVID-19 pandemic (March 2020), the United States has experienced striking increases in the unemployment rate, reaching 13.2% in April. Similarly, in Arizona, the unemployment rate jumped to over 13.5% in April. The unemployment rates have since declined both nationally and in Arizona but remain higher compared to February 2020. In November 2020 (the most recent data available), the national unemployment rate was 6.7%, while in Arizona the rate was 7.8%—the 10th highest unemployment rate among all U.S. states.


This brief summarizes the different types of food stores open in Camden, New Jersey and in a one mile radius around the city during 2008 to 2014.